Recurrent miscarriage/ RPL Recurrent Pregnancy Loss
If you are reading this first I’m sorry for what you have been through. The hardest days come when we lose hope or lose the chance for something we thought was coming. Dealing with this journey is not easy and the stress and emotions that come with it are a rollercoaster.
First give yourself permission to be sad/grieve and take comfort in what you have. Then after that time it always helped me to make a new plan, have a new start and think about the next steps.
It is hard to remain optimistic and positive in this journey and simultaneously you want to remain positive to improve chances, and worry if you are too negative and hopeless good things won’t come.
There are many reasons for miscarriage, and hopefully we can help clarify some of the anatomical causes that could be optimized.
A miscarriage, also known as spontaneous abortion, is a loss of pregnancy before the 20th week of gestation. Researchers think that about 10-25% of all pregnancies end up in miscarriage. Could there be a link between recurrent miscarriages and endometriosis?
What are the reasons someone may experience a miscarriage or recurrent miscarriage?
Genetic abnormality: the most common reason for early first trimester miscarriage is chromosomal abnormality. These are greatly influenced by maternal age due to change in egg quality as we age. These pregnancy abnormalities are caused by random chromosome errors in most cases. Many times patients can experience early miscarriage or chemical pregnancy and only see a delayed menstrual period. When patients are tracking their cycles and pregnancy tests closer they may notice these subtitles and early pregnancy failures are more common than one realizes. When you are going through infertility and closely tracking every day and ovulation, you are hyper aware of the cycle and the earliest pregnancy possibility. Our bodies naturally are capable in most cases of recognizing abnormal genetics in the fetus and if not compatible miscarrying something that isn’t right.
Even though this is devastating I like to encourage patients this is a sign your body knows what to do. There are even a few positives in this situation. 1. You underwent successful ovulation, fallopian tube pick up and fertilization. 2. The fallopian tubes work and transported the embryo successfully into the uterus. 3. The uterine lining was good enough to implant the embryo. 4. The body has error correction and tried to rectify what wasn’t right. That is actually no small feat!
Can autoimmune disease cause miscarriage or immunologic testing help me?
Yes! Autoimmune disease can cause recurrent pregnancy loss. A syndrome called Antiphospholipid syndrome can cause RPL in 8-42% of recurrent losses.
Antiphospholipid syndrome or aPL is defined by several different clinical and diagnostic criteria (some by history some by lab tests).
These include clinical history of a blood clot (deep vein thrombosis), a pregnancy complication in the past including one or more unexplained death of fetus after 10 weeks, pregnancy history of premature birth due to severe preeclampsia before the 34th week or three or more unexplained losses before 10 weeks with normal genetic analysis and no anatomic abnormality.
How do you diagnose aPL?
The labs used are lupus anticoagulant present on 2 different blood tests 3 months apart. Anticardiolipin antibody (IgG or IgM) in the mothers blood with a medium to high titer on again 2 different tests more than 3 months apart. Anti-Beta2 glycoprotein-I antibody again high on 2 or more blood tests 3 months apart.
The key here is it has to include one of the clinical factors and one of the laboratory tests which is positive 2 times more than 3 months apart.
Are there other immune factors which can impact miscarriage?
Researchers are studying the effects of CD16-NK or natural killer cell elevation and its role in pregnancy loss. Elevated blood cytokines, antibodies against the father and other alloimmune factors could cause difficulty in pregnancy. Screening for these is not necessarily recommended by ASRM however in someone with multiple losses an experienced physician on recurrent loss can be consulted. Reproductive immunologist examine these blood profiles and may follow a patient in pregnancy.
Can my hormones cause miscarriage?
Yes!
Hormonal effects from uncontrolled thyroid disease, conditions like uncontrolled diabetes or a prolactin elevation or tumor can cause miscarriage. We recommend a basic hormone panel to evaluate for any abnormality when trying and failing to get pregnant or experiencing multiple losses. Note these values are followed more rigidly while trying for fertility, pregnancy then they are in other times in life. This is why your routine primary care doctor or endocrinologist may use different levels of “normal.”
What other reasons can cause RPL or recurrent pregnancy loss?
Recurrent pregnancy loss or RPL is defined by American Society of Reproductive Medicine as 2 or more failed clinical pregnancies. Miscarriages can be recurrent due to various reasons. 15-25% of pregnancies can end in miscarriage. RPL occurs in only 5% of women with 2 losses and women with 3 or more losses in less than 1% of the population.
There are many factors that can increase the risk of miscarriage. These include advanced age (>40 years means rate of 50% or more), previous pregnancy loss, uterine anomalies, poor health conditions (e.g. uncontrolled diabetes, obesity), infections, stress, and smoking during pregnancy.
Can endometriosis increase the risk of miscarriages?
Endometriosis is the growth of endometrial-like tissue in areas of the body other than the uterus. Some of the ways in which endometriosis can affect fertility and contribute to miscarriage include:
- poor egg quality
- anatomical changes in the uterus and uterine lining
- scarring and adhesions in the fallopian tubes
- chocolate cysts in the ovaries
- inflammation due to high levels of cytokines
What does the research say?
Several studies have attempted to establish a consensus on the relationship between endometriosis and miscarriages.
For example, a 2016 study examined 478 pregnancies with histologically proven endometriosis and 964 unaffected pregnant women. It showed that the miscarriage rate was significantly higher in women with endometriosis (20%) than in the controls (12%). Those with a previous history of infertility had even higher miscarriage rates (50%) compared to those who didn’t (30%).
A meta-analysis of studies comparing pregnant women with endometriosis to those without, revealed that endometriosis can be a significant risk factor for miscarriages.
Similarly, another retrospective observational study in 268 pregnant women of reproductive age also showed higher rates of miscarriage in those with endometriosis (35.8%) compared to healthy controls (22%). The study concluded that superficial lesions in mild endometriosis can lead to an inflammatory situation that affects egg maturation, fertilization, and implantation.
What can I do to improve my chances of a healthy pregnancy?
If you experience severe pain with periods, pain with intimacy, or have difficulty conceiving, please seek advice early from a specialist.
If you have been through multiple miscarriages and have no explanation or have multiple miscarriages despite normal genetic embryos/fetus you may have endometriosis or another pelvic condition contributing.
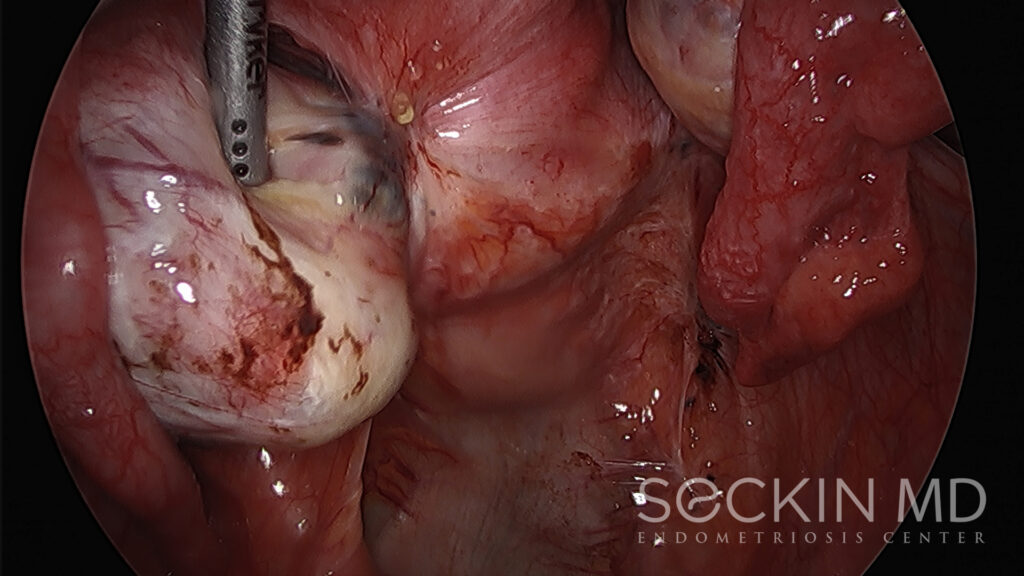
Most reproductive endocrinologists or fertility doctors feel they can bypass endometriosis with IVF. We however see many patients that have failed IVF or have multiple miscarriages even despite normal tested PGS embryos. These cases are difficult and a thorough inspection of the pelvic can be conducted with hysteroscopy, laparoscopy and evaluation and treatment of endometriosis or adhesions if there. Surgery with laparoscopic deep excision surgery may reduce the risk of miscarriage. Using this technique, a skilled surgeon can remove all visible and deep-infiltrating lesions and evaluate the uterus. Surgery can also help reduce inflammation and restore anatomy.
We have seen many patients go on to have healthy normal pregnancies following the surgery.
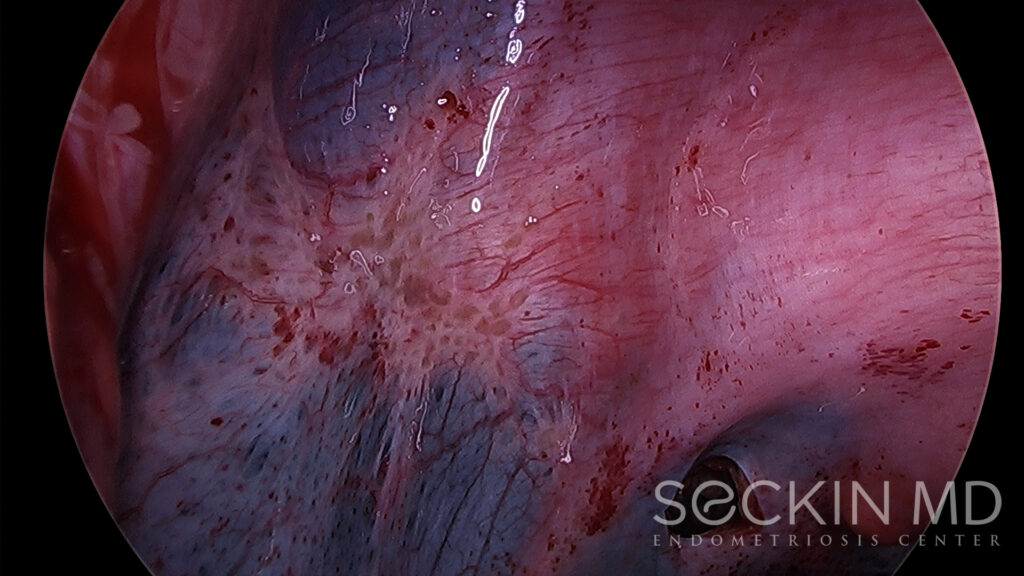
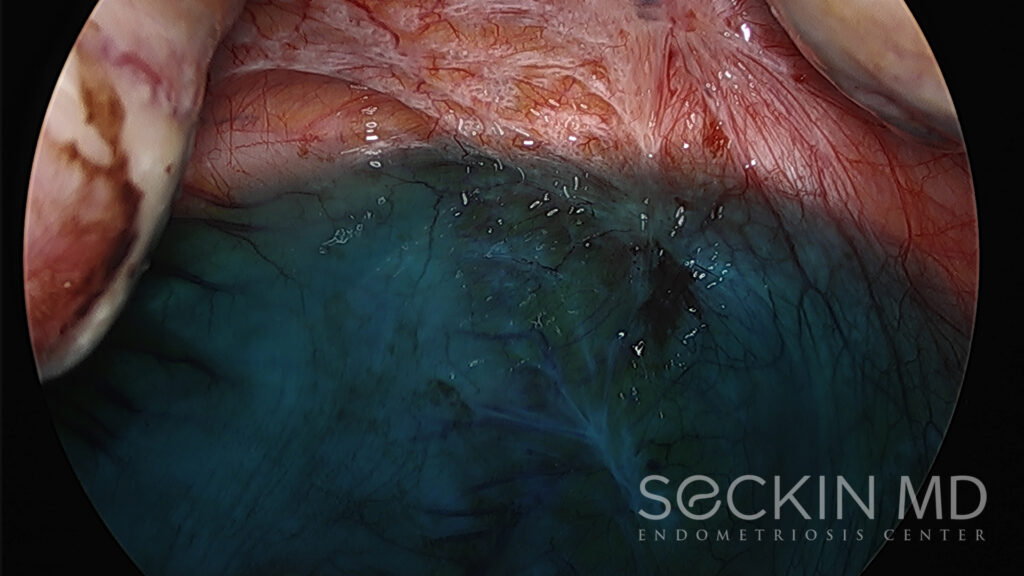
Below you will see examples of patients with seemingly normal imaging and multiple miscarriages and the endometriosis found in their pelvis on laparoscopic evaluation.